No one really signs up for surgery with a grin on their face. Whether it’s something small like a nagging hernia or something that carries a bit more emotional weight, like a tumor that needs removing — that pre-surgery wait brings its own brand of tension. It’s not just about being brave under the knife. It’s about trusting that the person holding the scalpel knows exactly what they’re doing. That the healing won’t just be physical, but emotional too.
And in today’s world, surgery looks a whole lot different than it did a decade or two ago. We’ve come a long way — less cutting, faster recovery, more precision, and a better patient experience overall. That’s the beauty of minimally invasive general surgery — it’s changing how people heal, inside and out.
Let’s Start with the Basics: Surgery, but Smarter
Gone are the days when any surgical issue meant a massive incision and a week-long hospital stay. Now, many general surgeries are performed through small keyhole-sized incisions. Surgeons insert a camera and specialized tools, and they do the job while watching everything in real-time on a high-definition screen.
It sounds high-tech — and it is. But at the heart of it is a very human goal: to fix what’s wrong while disturbing your body as little as possible.
This approach is especially useful in procedures involving the gallbladder, intestines, appendix, and yes, even hernias. The outcomes? Less blood loss, reduced risk of infection, quicker healing, and a better shot at getting back to life without missing a beat.
Hernias Happen — And They’re More Common Than You’d Think
Let’s talk about the elephant in the room — the humble but incredibly annoying hernia. A weak spot in the muscle wall that lets something sneak through (like intestine or tissue). You might notice a lump or feel discomfort when you cough, bend, or lift something heavy.
They’re not usually dangerous right away, but left untreated? They can cause some serious complications.
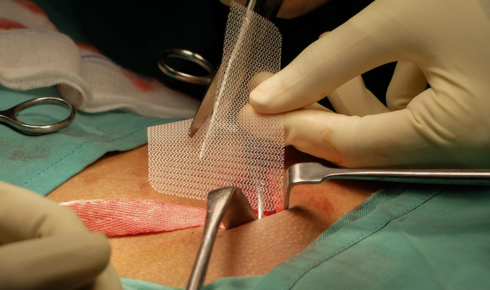
Getting hernia surgery is often the recommended route — especially if the hernia is growing or causing pain. And nowadays, most hernia repairs are done laparoscopically. That means smaller incisions, quicker recovery, and way fewer “ouch” moments when you laugh or sneeze the next day.
A good surgeon will walk you through the options — mesh or no mesh, open or minimally invasive, general or local anesthesia. The more you understand, the more empowered you’ll feel walking into that operating room.
When It’s More Serious: Tumor Removal and the Emotions That Come With It
The word “tumor” has a way of tightening the air in a room. It’s scary. It’s unknown. And whether it’s benign or malignant, the emotional weight is real.
Tumor removal surgery can range from very simple (a small lump under the skin) to incredibly complex (involving vital organs or major tissue removal). Sometimes it’s the first step in diagnosis. Sometimes it’s part of a larger treatment plan.
What matters most — beyond the technique — is how your surgical team handles the journey. Do they listen? Explain? Reassure? Answer the same question three times without making you feel silly?
The best surgeons understand they’re not just removing tissue — they’re helping people reclaim peace of mind. That’s a powerful responsibility.
Why Minimally Invasive Isn’t Just a Buzzword
If there’s one phrase that comes up again and again in modern surgery, it’s minimally invasive general surgery. And while it might sound like marketing speak, it’s actually a real shift in how medicine operates (literally and philosophically).
Instead of “cut it open, fix it, sew it shut,” the mindset now is: “How can we fix this with the least disruption possible?”
Smaller incisions mean smaller scars. But they also mean less trauma to internal structures. That’s what allows people to go home the same day, eat normal food sooner, and even get back to light activity within days instead of weeks.
Of course, not every case qualifies for a minimally invasive approach. But if you’re a candidate, it’s worth asking about — and worth choosing a surgeon who’s experienced in these techniques.
What Healing Actually Looks Like
TV shows love to fast-forward surgery recovery. One moment you’re in the hospital, next thing you know, you’re walking around like nothing happened. Real life? A bit messier.
There’s the fog from anesthesia, the slow shuffle on day two, the awkward moment when you realize laughing still hurts. There’s discomfort, but also hope. Progress. A return to normal, one small win at a time.
One day you wake up and realize — the fear is gone. The scar’s fading. And you feel strong again.
Final Thoughts: You’re More Than a Patient
Surgery isn’t just a medical event. It’s a deeply personal experience — one that requires vulnerability, trust, and strength. Whether you’re preparing for a routine hernia repair or something more complex like tumor removal surgery, remember this: you’re allowed to ask questions. You’re allowed to feel scared. And you deserve to feel safe.
Choose a surgeon who sees you. Not just your condition. One who values communication as much as they value precision. And if you have access to minimally invasive general surgery, explore it. It might just change the way you heal — and the way you feel about surgery in general.
Because the truth is, modern surgery isn’t just about better tools — it’s about better care. The kind that understands you’re not just trying to survive the procedure. You’re trying to get back to living.